MENU
Follow Us
Specializing in fertility, hormone health, and chronic conditions. For those looking for personalized care, especially when conventional options haven’t brought full relief, we blend Traditional Chinese Medicine with evidence-informed care to help you get to the root, support your body, and finally start feeling better.
Modern healthcare designed to treat the whole you — not just the symptoms.
How our vaginal health program Savvy Vagi utilizes evidence-informed treatments
The vagina is a self-cleaning, self-regulating organ that is composed of many different flora, or positive bacterial organisms, that help balance the pH, fight off infection, and influence your uterine health.
The numbers don’t lie, and the high numbers of recurrent infections, unresolved symptoms, and chronic vaginal concerns all stem from a misalignment between treating the problem and setting up your vaginal microbiome for success. Your vaginal microbiome should be resilient and largely self-regulating; a healthy microbiome can fight off potentially harmful disruptions that naturally occur. That’s why we focus on understanding where your microbiome might need additional support and how to reset your microbiome’s make-up naturally and comfortably.
When you come to Eau Claire Acupuncture for vaginal symptoms or concerns, we have a few specific goals in mind:
- Resolve your symptoms naturally
- Improve vaginal comfort
- Restore your vaginal microbiome to prevent frequent recurrence of infections or symptoms
- Rebuild vaginal tissue thickness and hydration to reinforce the body’s natural protective barrier.
- Address digestive microbiome imbalance that may be impacting vaginal health (this can be very common if you have been prescribed oral antibiotics continually for vaginal infections)
Any symptom you may have can play a part in the story of your health. Plus, your fertility and pregnancy can be impacted by your vaginal microbiome. Even if you are not having classic bacterial vaginosis symptoms, you may have an imbalance that is affecting your ability to conceive or stay pregnant or are just curious about your microbiome for your fertility or pregnancy journey, starting with a free consultation is easy and informative! Your free consultation can be a great way to speak to your provider and understand if Savvy Vagi might be a good fit for you.
What is the vaginal microbiome?
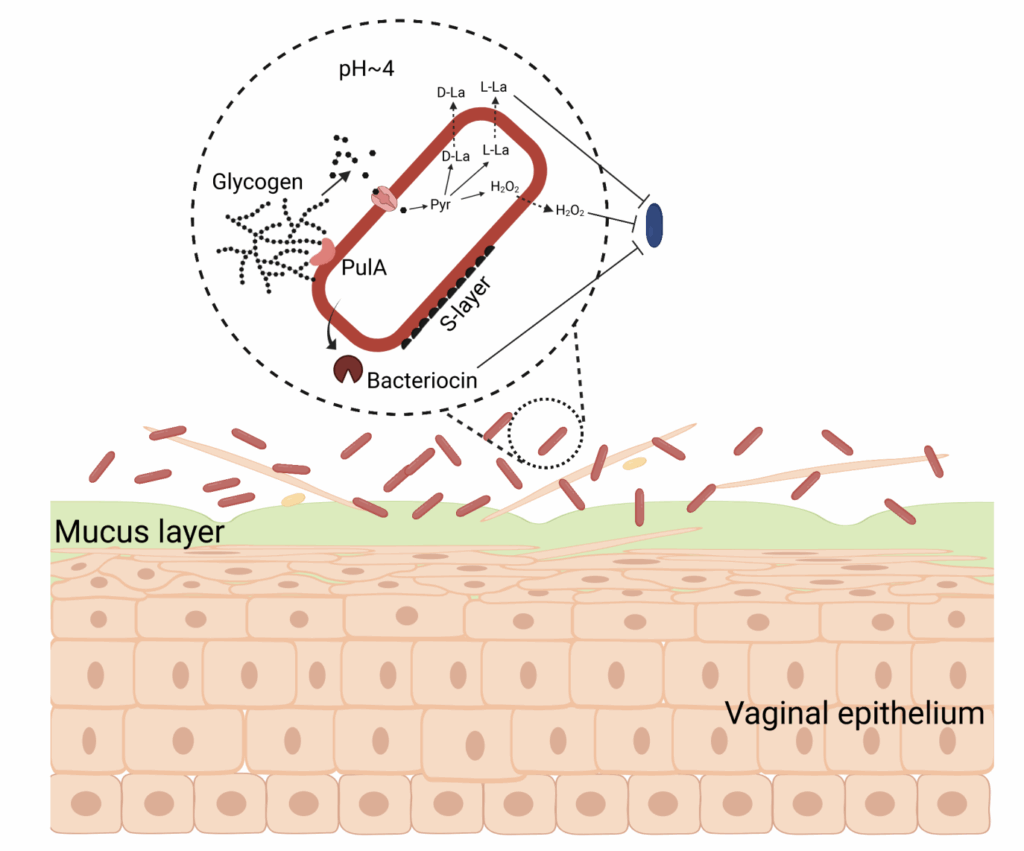
The vaginal microbiome is a community of positive bacterial species that produce lactic acid, maintaining the vaginal pH as acidic. The acidic pH of the vagina helps to fight off infections or pathogens that enter the vagina. Lactobacillus species produce the lactic acid that is essential for strong pH maintenance. When antibiotics are introduced, because they are non-selective, the Lactobacillus community can be killed off alongside the negative bacteria causing symptoms. This can lead to the vagina’s pH becoming basic, rather than acidic, making it more prone to reinfection.
A Lactobacillus dominated vaginal microbiome has long been considered the healthiest, most resilient environment. Lactobacillus are the group of positive bacterial species that occupy and make up the lining of your vagina, as well as your digestive tract. They exist in your vagina’s mucus layer and some adhere to your epithelial cells that make up the “skin” of your vagina.
There are different types of healthy vaginal microbiomes, which are defined by the species of bacteria that is most prevalent (Martin & Marazzo, 2016). Testing of your vaginal microbiome can tell us what type your microbiome falls into, and if said type can be more likely to be at risk of transmitting a vaginal infection. For example, high community diversity can make your vagina more susceptible to BV (Martin & Marazzo, 2016). BV is associated not only with negative vaginal symptoms, like itching, burning, inflammation, and abnormal discharge, but has also been associated with gynecologic cancer and increased risk of STIs (Gillet et al., 2012).
This cellular level depiction of the microbiome can help you visualize what makes up the different layers of your vagina. Positive and negative bacteria make up the mucus layer, and can even adhere to the skin layer.
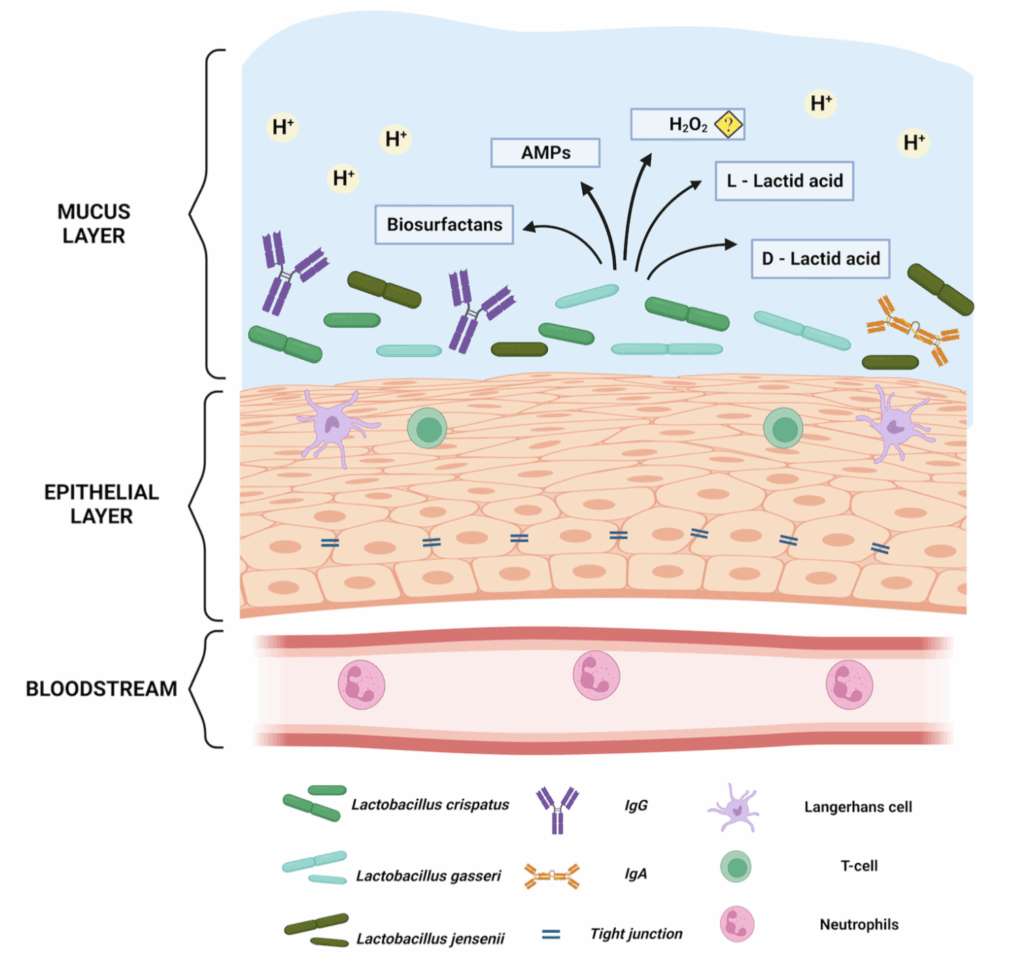
Microorganisms. 2023 Mar 1;11(3):636. doi: 10.3390/microorganisms11030636
How are vaginal infections commonly treated?
Oftentimes, vaginal infections or vaginal symptoms are treated with antibiotics. Or, you may even try an over the counter remedy for yeast infections or general vaginal discomfort. One third of women are estimated to ineffectively self-diagnose a yeast infection, meaning over the counter options are oftentimes ineffective and allow the true infection to go unaddressed (Ambizas, 2015). Furthermore, because these methods are usually non-specific to the type of microbiome someone has, the results can be negligible or lead to recurrence of symptoms down the line.
Prescription antibiotics are usually the most common treatment option your gynecologist will recommend if you present with vaginal infection symptoms. An oral antibiotic commonly used to treat bacterial vaginosis (BV), called metronidazole, was investigated for recurrence of symptoms after a round of antibiotic treatment.
- It was found that 58% of women experienced a recurrence of BV within 12 months of their treatment, and 69% had a disruption in their vaginal flora markers (Bradshaw et al., 2006).
- Another common antibiotic, trinadizol, has a 20-40% rate of recurrence within 1-2 months (Amabebe et al., 2025).
With antibiotic treatment being such a common prescribed treatment, vaginal flora health can be affected, as well as digestive health (Lathakumari, 2024). A disrupted digestive microbiome equilibrium can cause problems with metabolic homeostasis, immunity, and metabolism (Lathakumari, 2024). Therefore, natural solutions, rather than antibiotic treatment as a first line to BV, reduces your risk of digestive upset. We consider whole person symptoms such as digestive symptoms you report alongside vaginal concerns, to get the big picture of your health, and understand how previous BV treatments might be impacting your current situation.
Another factor to consider is aerobic vaginitis, which can be often misdiagnosed as bacterial vaginosis. Antibiotics that target BV anaerobes (which need an oxygen deprived environment) don’t work against the aerobes, like E. Coli or strep strains, that can infect areas of the vagina that have more oxygen present (Donders et al., 2002).
Yeast infections are another common condition that can be misdiagnosed and treated with the incorrect prescription. Clinical guidelines recommend < 6 months of anti-yeast (fluconazole) treatment for recurrent yeast infections; yet, reinfection occurs in up to 50% of women (Neal et al., 2022). Although common anti-fungals can control the yeast infection, long-term eradication fails (Sobel et al., 2004).
Determining the exact cause of your vaginal infection — whether that be yeast, aerobic bacteria, anaerobic bacteria, or simply an imbalance of beneficial microbes in the vagina — is key to generating the correct treatment. Because we test for over 2,000 microbes, our results can help pin down the very specific, cellular make-up in your vagina.
How does my vaginal health impact my pregnancy?
Certain bacterial species have been associated with pregnancy safety concerns, such as preterm birth, low birth weight, neonatal infections, postpartum endometritis, and late miscarriage (Fettweis , 2019). These bacterial species are most often the species that cause BV; therefore, BV is often coined as a causative factor in these conditions. Furthermore, for women undergoing IVF, BV has been associated with increased risk for miscarriage in the first trimester (Ralph, 1999), indicating the need for vaginal microbiome emphasis in all forms of conception planning.
Unresolved vaginal infections can also impact fetal health during pregnancy. For example, amniotic infections have been found to frequently mirror the infection found in the vagina, indicating that infections in the vagina can ascend into the uterus (Romero, 2019). Also, vaginal infections can often lead to increased inflammatory cytokines during pregnancy and labor; these inflammatory cytokines can trigger pre-term birth as well as pre-term ruptured membranes (Cheng, 2025). Negative microbes in the vagina also act on the cervix to increase inflammation, weakening the barrier the cervix normally provides in healthy vaginas, acting as another mechanism to pre-term birth (Tantengco, 2022).
Savvy Vagi was not only created as a natural alternative to antibiotics, but also as an important factor in fertility. As a fertility specialist, Eau Claire Acupuncture and its providers, look at both the big and small picture when it comes to fertility and pregnancy.
Having vaginal symptoms during pregnancy or interested in ways that the vaginal microbiome might be impacting your fertility journey? Speak to Vallie, your vaginal health expert, to see if you might benefit from vaginal microbiome testing.
How does menopause impact my vaginal health?
Changes in estrogen and progesterone levels during and after menopause impact the lining of the vagina and uterus. Because these linings are where much of the vaginal microbiome resides, hormonal changes can significantly affect the vaginal microbiome. Furthermore, many women during or after menopause report vaginal dryness and other vulvovaginal symptoms, which are often attributed to menopause alone. However, the vaginal microbiome plays an important role both before and after menopause. Therefore, we recommend that women of any age consider vaginal microbiome testing to better understand their individual microbiome composition.
Estrogen helps promote the production of glycogen, an energy reserve that feeds Lactobacillus species in the vagina. When estrogen levels decline during menopause, Lactobacillus levels may decrease, leading to a more basic (higher pH) vaginal environment. As a result, post-menopausal women are at a higher risk of developing bacterial vaginosis (BV) and may experience more pronounced dysbiosis-related symptoms, particularly if prescribed antibiotics (Łaniewski, 2022).
DOI: 10.1038/s41564-022-01083-2
In addition, post-menopausal women often experience Genitourinary Syndrome of Menopause (GSM). Vaginal and vulvar symptoms may include burning, dryness, painful sex, and vaginal thinning. Sexual symptoms can include pain during or after intercourse, reduced lubrication, and vaginal dryness, as well as microtears caused by decreased vaginal wall thickness. Urinary symptoms may include frequent or urgent urination, burning with urination, recurrent urinary tract infections (UTIs), and stress incontinence.
All of these symptoms can be exacerbated when a vaginal infection is present and symptoms are misdiagnosed as GSM.
Interestingly, “the 20–50% of postmenopausal women with a Lactobacillus-dominated vaginal microbiome have a lower prevalence of GSM symptoms… altering the vaginal microbiome with estrogen or Lactobacillus supplementation could be considered as a treatment option for GSM” (Park, 2023).
Although research into microbiome-related reduction of GSM symptoms is ongoing, early evidence suggests links between a healthy vaginal microbiome and reduced GSM symptoms. Resetting the vaginal microbiome and reducing harmful bacteria may be important first steps in managing post-menopausal symptoms that are often dismissed as a normal part of aging. We can also help recommend safe products to manage symptoms, ensuring your self-care routine supports vaginal balance while effectively addressing discomfort.
Start with your free consultation to talk with your provider about your symptoms, because we believe that all ages can benefit from vaginal health awareness and support.
Written by: Leandra O’Connell
References
Amabebe, E., Tatiparthy, M., Kammala, A. K., Richardson, L. S., Taylor, B. D., Sharma, S., & Menon, R. (2025). Vaginal pharmacomicrobiomics modulates risk of persistent and recurrent bacterial vaginosis. npj Biofilms and Microbiomes, 11(1), 115. https://doi.org/10.1038/s41522-025-00748-0
Bradshaw, C. S., Morton, A. N., Hocking, J., Garland, S. M., Morris, M. B., Moss, L. M., Horvath, L. B., Kuzevska, I., & Fairley, C. K. (2006). High recurrence rates of bacterial vaginosis over the course of 12 months after oral metronidazole therapy and factors associated with recurrence. The Journal of Infectious Diseases, 193(11), 1478–1486. https://doi.org/10.1086/503780
Cheng, D., Li, N., Sun, Q., Wang, K., & Gao, F. (2025). Vaginal microbiome and preterm birth: Composition, mechanisms and microbiota-directed therapies (Review). International Journal of Molecular Medicine, 56(6), 203. https://doi.org/10.3892/ijmm.2025.5644
Donders, G. G., Vereecken, A., Bosmans, E., Dekeersmaecker, A., Salembier, G., & Spitz, B. (2002). Definition of a type of abnormal vaginal flora that is distinct from bacterial vaginosis: aerobic vaginitis. BJOG: an international journal of obstetrics and gynaecology, 109(1), 34-43.
Fettweis, J. M., Serrano, M. G., Brooks, J. P., Edwards, D. J., Girerd, P. H., Parikh, H. I., … Buck, G. A. (2019). The vaginal microbiome and preterm birth. Nature Medicine, 25(6), 1012–1021.
France, M., Alizadeh, M., Brown, S., Ma, B., & Ravel, J. (2022). Towards a deeper understanding of the vaginal microbiota. Nature microbiology, 7(3), 367-378.
Gillet, E., Meys, J. F., Verstraelen, H., Verhelst, R., De Sutter, P., Temmerman, M., & Vanden Broeck, D. (2012). Association between bacterial vaginosis and cervical intraepithelial neoplasia: Systematic review and meta-analysis. PLOS ONE, 7(10), e45201. https://doi.org/10.1371/journal.pone.004
Lathakumari, R. H., Vajravelu, L. K., Satheesan, A., Ravi, S., & Thulukanam, J. (2024). Antibiotics and the gut microbiome: Understanding the impact on human health. Medicine in Microecology, 20, 100106.
Łaniewski, P., & Herbst-Kralovetz, M. M. (2022). Connecting microbiome and menopause for healthy ageing. Nature Microbiology, 7(3), 354–358. https://doi.org/10.1038/s41564-022-01071-6
Martin, D. H., & Marrazzo, J. M. (2016). The vaginal microbiome: Current understanding and future directions. The Journal of Infectious Diseases, 214(Suppl_1), S36–S41.
Neal, C. M., & Martens, M. G. (2022). Clinical challenges in diagnosis and treatment of recurrent vulvovaginal candidiasis. SAGE Open Medicine, 10, 20503121221115201.
Park, M. G., Cho, S., & Oh, M. M. (2023). Menopausal changes in the microbiome—A review focused on the genitourinary microbiome. Diagnostics (Basel), 13(6), 1193.
Pendharkar, S., Skafte-Holm, A., Simsek, G., & Haahr, T. (2023). Lactobacilli and their probiotic effects in the vagina of reproductive age women. Microorganisms, 11(3), 636. https://doi.org/10.3390/microorganisms11030636
Ralph, S. G., Rutherford, A. J., & Wilson, J. (1999). Influence of bacterial vaginosis on conception and miscarriage in the first trimester: Cohort study. BMJ, 319(7204), 220–223.
Romero, R., Gomez-Lopez, N., Winters, A. D., Jung, E., Shaman, M., Bieda, J., Panaitescu, B., Pacora, P., Erez, O., Greenberg, J. M., Ahmad, M. M., Hsu, C. D., & Theis, K. R. (2019). Evidence that intra-amniotic infections are often the result of an ascending invasion—A molecular microbiological study. Journal of Perinatal Medicine, 47(9), 915–931.
Sobel, J. D., Wiesenfeld, H. C., Martens, M., Danna, P., Hooton, T. M., Rompalo, A., … & Chu, T. C. (2004). Maintenance fluconazole therapy for recurrent vulvovaginal candidiasis. New England Journal of Medicine, 351(9), 876-883.
Tantengco, O. A. G., & Menon, R. (2022). Breaking down the barrier: The role of cervical infection and inflammation in preterm birth. Frontiers in Global Women’s Health, 2, 777643. https://doi.org/10.3389/fgwh.2021.777643
Brand photography by Christy Janeczko
Copywriting by The Copy Shift
|
Follow Us
Hours:
Tuesday 9-7
Wednesday 9-7
Thursday 9-7
Friday 9-4
info@eauclaireacu.com
call or text
(715) 575-1220
323 E Madison St, Eau Claire, WI 54703
Book Your Appointment
We blend Traditional Chinese Medicine with evidence-informed care to help you get to the root, support your body, and finally start feeling better.